 Found a word you're not familiar with? Double-click that word to bring up a dictionary reference to it. The dictionary page includes an audio sound file with which to actually hear the word said. Found a word you're not familiar with? Double-click that word to bring up a dictionary reference to it. The dictionary page includes an audio sound file with which to actually hear the word said. |
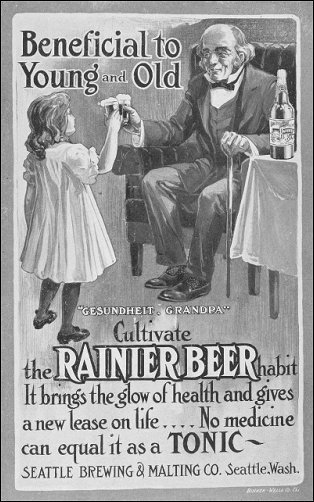 Right: changing times: oversight and claims for medicines have improved somewhat since this early 1900s advertisement appeared in newspapers.
Right: changing times: oversight and claims for medicines have improved somewhat since this early 1900s advertisement appeared in newspapers.
 Further implications
Further implications
Though supporters claim that banning the over-the-counter sale of codeine products will be a significant step toward addressing Australia's problems with therapeutic drug misuse, there is a general acknowledgement that this step is only a small part of the solution.
One of the concerns raised by the impending ban on the over-the-counter sale of codeine is that there will not be adequate support available for those suffering withdrawal symptoms when their access to the drug is reduced or ended.
Suzanne Nielsen, a senior research fellow at the National Drug and Alcohol Research Centre (NDARC), has indicated that more funding will be needed to treat those withdrawing from the addictive drug.
Ms Nielsen stated, 'There is (sic) going to have to be dedicated funds and treatment services allocated to respond to this problem.' She has warned that mass withdrawals could be a particular problem in regional areas where codeine product use tends to be relatively higher and where there are already inadequate support facilities.

It has also been noted that the problem of therapeutic opioid addiction does not simply involve over-the-counter medications.
Research from the Penington Institute in 2016 showed 71 per cent of overdose deaths in Australia were due to prescription medications. The National Drug and Alcohol Research Centre has stated that around 800 Australians a year die from prescription drug overdoses, particularly opioids, including codeine, fentanyl, methadone and morphine. Australia ranks eighth in the world's top 30 users of prescription painkillers such as these.

An opinion piece published in The Australian Family Physician in December 2016 noted the importance of doctors prescribing carefully, advising patients on pain management and monitoring their use of addictive medications. It stated, 'Prescription drug abuse is a complex problem that needs to be addressed by society and the medical profession together. Doctors need to be aware of the risk of dependence and overdose with any drugs they prescribe, but particularly drugs of dependence. Opioids and benzodiazepines are associated with the highest risk of overdose deaths... In a general practice setting, the use of evidence-based guidelines can help with managing inappropriate requests for drugs of dependence.'

Critics of the ban on over-the-counter sales of codeine products have argued that the problem of codeine misuse will not be solved by placing responsibility on prescribing doctors who do not always exercise it effectively.
One of the solutions proposed is to implement a real-time monitoring scheme which would enable any doctor to check when a particular patient was last prescribed an addictive drug.
Suzie Kanis, whose son died of a prescription drug overdose has criticised doctors' failure to coordinate their treatments and regretted the lack of a monitoring system that would help them do so.
Mrs Kanis stated, ' Why did the doctors not check what medication they were each giving him?' She believes her son's death highlights the need for an electronic real-time prescription monitoring system that would alert doctors to the particular mix of drugs a patient had been prescribed.

On January 19, 2018, the Therapeutic Goods Administration released a discussion paper titled ' Prescription strong (Schedule 8) opioid use and misuse in Australia - options for a regulatory response' to consider the need for greater regulation of these prescribed drugs.

Beneath the question of how Australia regulates its therapeutic use of opioids is the larger question of how we manage pain. Australia's National Pain Strategy has as its goals: people in pain as a national health priority; knowledgeable, empowered and supported consumers; skilled professionals and best-practice evidence-based care; access to interdisciplinary care at all levels; quality improvement and evaluation and ongoing research. Critics argue that though there have been some improvements, the country has a long way to go.

